Crohn’s Disease:
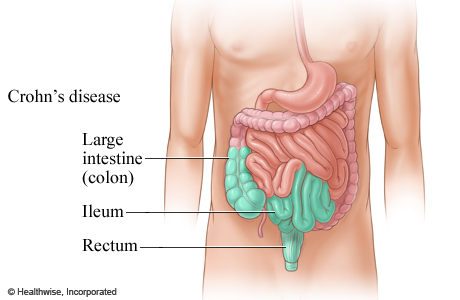
Crohn’s disease can affect any part of the digestive tract.
It primarily causes abdominal pain, diarrhea (which may be bloody if inflammation is extreme), vomiting, or weight loss, but may also cause complications outside the gastrointestinal tract such as skin rashes, arthritis, inflammation of the eye, tiredness, and lack of concentration.
Crohn’s disease can be in multiple places in the digestive tract at the same time.
Crohn’s is considered one of the main causes of Short Bowel Syndrome.
Sign’s & Symptoms
Diarrhea:
Individuals with Crohn’s disease often encounter frequent loose or watery bowel movements. The stool may occasionally contain thick, dark blood, distinct from the bright red smears associated with bleeding hemorrhoids. Unlike cases of ulcerative colitis, there is typically less mucus or pus in the stool.
Pain:
Patients may endure crampy, achy, or sharp pain in the affected area. Most commonly, those with Crohn’s disease experience pain on the lower right side of the abdomen (lower right quadrant) and just below the bellybutton. This is primarily because the terminal ileum, where the small intestine meets the large intestine, is often involved in Crohn’s disease cases. The terminal ileum crosses from left to right just above the beltline and connects with the large intestine in the lower right quadrant.
The nature of the pain associated with Crohn’s disease varies based on the affected part of the gastrointestinal (GI) tract. Sharp pain is typically linked to disease in the terminal ileum, while crampy pain, similar to that of ulcerative colitis, is associated with disease in the colon. Pain may be temporarily relieved after a bowel movement.
Fever:
Crohn’s disease is characterized by inflammation, and fever is a key feature of the inflammatory process (alongside pain, swelling, and redness). Some individuals with Crohn’s disease experience a high fever, particularly during the acute phase of a flare-up. Others may have a persistent, low-grade fever. Fever may be accompanied by irritability and fatigue. In some cases, the fever recurs daily, especially late in the day, breaking repeatedly during sleep and causing night sweats.
Signs and Symptoms Unrelated To The GI Tract
Crohn’s disease can manifest with signs and symptoms beyond those affecting the gastrointestinal tract. These non-GI symptoms may coincide with intestinal issues or precede them by weeks or even months. If your healthcare provider suspects inflammatory bowel disease, they will inquire about the presence of additional symptoms, such as:
- Redness and inflammation of the eye (iritis)
- Joint pain, often in larger joints like knees, ankles, elbows, wrists, and shoulders, with potential migration from one joint to another (migrating arthralgia)
- Skin lesions, including tender red nodules on the shins or calves (erythema nodosum)
- Mouth sores (aphthous ulcers)
Causes
Described as an “idiopathic” condition, Crohn’s disease involves inflammation as part of the body’s immune response. Typically, an immune response is triggered by a specific factor, but, as of now, no definitive “trigger” has been identified for the inflammatory response observed in Crohn’s disease.
Genetics may play a role in Crohn’s disease, although it doesn’t exhibit a straightforward correlation from parent(s) to offspring. The condition tends to have a familial pattern, with as many as 20 to 25 percent of Crohn’s disease patients having a relative diagnosed with either Crohn’s disease or ulcerative colitis. Certain ethnic groups also show a higher incidence.
Moreover, potential environmental factors have been associated with initial episodes or relapses. Crohn’s disease seems to predominantly affect individuals in Western, industrialized societies. However, whether this is linked to environmental conditions or dietary factors remains undetermined.
Diagnosis
The individual is expected to undergo various laboratory tests and possibly undergo one or more imaging procedures, enabling the doctor to visually assess the condition of the intestine. Laboratory tests comprise blood tests and stool cultures, which help evaluate the inflammatory process and offer insights into the underlying cause. Three prevalent imaging procedures are employed— one involving X-rays and the others utilizing endoscopy, allowing the physician to directly examine the internal structures.
Additional forms of imaging studies encompass:
- Sigmoidoscopy
- Colonoscopy
- Barium enema
These studies play a crucial role in determining the specific type of Crohn’s Disease affecting the patient.
Types of Crohn’s Disease
Gastroduodenal Crohn’s Disease (CD) is a condition that impacts the stomach and the duodenum, commonly leading to misdiagnosis as ulcer disease. Accurate diagnosis often occurs only after failed ulcer treatments or when Crohn’s disease is identified in other parts of the gastrointestinal tract. Symptoms of gastroduodenal CD include appetite loss, weight loss, nausea, upper-middle abdominal pain, and vomiting.
Jejunoileitis is a manifestation of Crohn’s disease affecting the jejunum, the longest portion of the small intestine. Symptoms encompass abdominal pain and cramps after meals, diarrhea, and malnutrition due to nutrient malabsorption in the jejunum. Fistulas, abnormal openings in the intestinal tract, may form, linking the diseased area to other parts of the intestine or organs, posing an increased risk of infections outside the GI tract.
Ileitis targets the ileum, the last part of the small intestine, resulting in symptoms such as diarrhea, cramping, and pain in the right lower quadrant and periumbilical area, particularly after meals. Vitamin B12 malabsorption can lead to peripheral neuropathy, while folate deficiency may hinder red blood cell development, increasing the risk of anemia. Fistulas and inflammatory masses can also develop.
Ileocolitis is the most prevalent type of Crohn’s disease, affecting both the ileum and the colon. The diseased area of the colon is often contiguous with the diseased ileum, involving the ileocecal valve. However, in some cases, non-contiguous areas of the colon may be affected. Symptoms mirror those of ileitis, with weight loss being a common feature.
Crohn’s Colitis, also known as Granulomatous Colitis, specifically targets the colon. It differs from ulcerative colitis in two key ways: the presence of healthy tissue between diseased areas and the potential sparing of the rectum, manifesting only in the colon. Ulcerative colitis, in contrast, is always continuous and affects both the rectum and areas beyond.
Treatment
Medical management of Crohn’s disease focuses on reducing symptoms and bringing on a remission. Once this is accomplished, the goal is to maintain remission for as long as possible. Most of the medications used to treat Crohn’s disease are generally safe for long-term use. Many doctors keep individuals on maintenance doses of medications indefinitely.
Medications commonly used to treat Crohn’s disease include:
- 5-ASA compounds
- Steroids
- Medications that suppress the immune system
- Antibiotics
- Infliximab (Remicade)
- Experimental treatments
- Alternative treatments
References
Health Information Publications (C) 2002-2011
http://ehealthmd.com/library/crohnsdisease/CD_whatis.html
http://ehealthmd.com/library/crohnsdisease/CD_symptoms.html
http://ehealthmd.com/library/crohnsdisease/CD_causes.html
http://ehealthmd.com/library/crohnsdisease/CD_diagnosis.html
http://ehealthmd.com/library/crohnsdisease/CD_types.html
http://ehealthmd.com/library/crohnsdisease/CD_treatment.html
